Your rights and Quality of Care
Clinical Governance Framework
Euroa Health Inc (EHI) will ensure consumer participation, clinical effectiveness, an effective workforce and risk management through a robust Clinical Governance System consisting of:
- Clear definition of roles and responsibilities across the organisation
- Clear priorities and strategic direction
- Compliance with legislative and regulatory requirements
- Committee and Organisational structure and processes
- Policies and procedures based on evidence-based best practice
- Transparent planning and allocation of resources to achieve goals
- Just culture allowing the organisation to learn from incidents and near misses improving patient
- safety and continuous quality improvements
- Measure, monitor, evaluate and improve organisational and clinical performance, quality and safety
- Continuity of care across the health spectrum
- Ongoing participation and feedback from consumers, community, service providers and staff
Euroa Health Inc (EHI) is guided by the Department of Health’s clinical governance policy framework which outlines four domains of clinical governance:
- Consumer participation
- Clinical effectiveness
- An effective workforce
- Risk management (encompassing incident reporting and management)
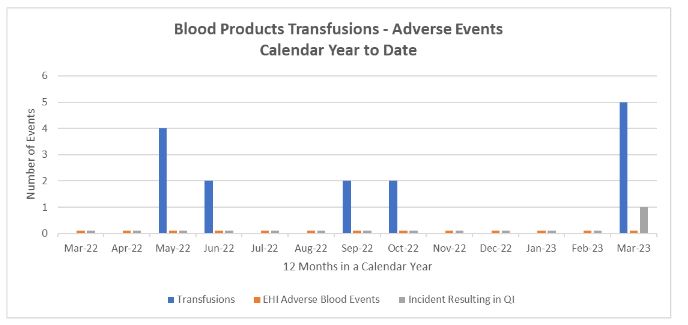
Euroa Health Board Subcommittees of the support and monitor implementation of quality and safety and participate in decision making. The operational committees ensure a systems approach to improving quality and performance; a cyclical model is used, which includes the following elements: monitoring, assessment, action, evaluation, and feedback. The Euroa Health Subcommittees can be seen below.
Image 1. Euroa Health Board Subcommittees
The Risk Management Framework and Risk Register assist staff to apply a consistent and comprehensive approach to risk management by identifying, analysing, evaluating, and treating risks. The Board has adopted Risk Management as an integral component of Clinical and Corporate Governance and Strategic direction. Successful risk management results in improved efficiency of operations, enhanced strategic direction, continuous quality improvement and assurance to stakeholders regarding EHI’s ability to manage risks and make decisions open and transparently.
Image 2. Model of Risk Analysis undertaken at Euroa Health.

The objectives of the risk management framework are to:
- Provide a systematic approach to the early identification and management of risks.
- Provide consistent risk assessment criteria.
- Make available accurate and concise risk information that informs decision making including business direction.
- Adopt risk treatment strategies that are cost-effective and efficient in reducing risk to an acceptable level.
- Monitor and review risk levels to ensure that risk exposure remains within an acceptable level.
EHI has a system to manage incident reporting, investigations, and management. Sentinel events are reported to the Sentinel event program (Department of Health), and a root cause analysis is conducted when required. All staff are accountable for identifying and reporting incidents and initiating quality improvements. Results are evaluated by the managers; incidents are trended and reviewed by the Quality and Risk Committee.
Acute Patient Outcomes
As part of our quality framework, we regularly measure ourselves against a range of ‘Clinical Indicators’.
Hand Hygiene
Hand hygiene (or hand washing) is one of the best ways to stop infections so, as a priority, we educate and train all caregivers in the World Health Organisation’s (WHO) “five moments” for hand hygiene.
Our Infection Prevention Nurse and audit team complete compliance audits on a regular basis.
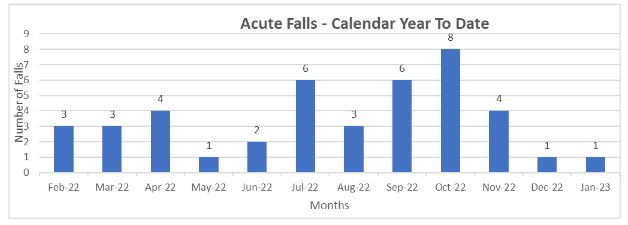
Patient Falls
A fall in a hospital is when a patient suddenly and unintentionally falls to the ground. This can happen in a hospital setting for several reasons, such as a change in medication or just because the surroundings are unfamiliar. Falls can injure patients and affect their recovery and independence.
We achieve a lower rate through our established Falls Prevention and Management Program and an electronic Incident/Risk Management and Reporting System. A variety of best practice tools and prevention intervention guidelines are utilised to identify those patients/consumers at high risk of having a fall. This graph shows the number of falls over the past year.
Pressure Injuries
A pressure injury is an area of damage to the skin and underlying tissue caused by constant pressure or friction. This can sometimes occur when a patient is in one position and unable to easily move for a long period.
Pressure injuries can be prevented. We also help to reduce the likelihood of our patients developing pressure injuries during their hospital stay, by assessing their individual risk and follow individual care plans.
As part of our clinical care, we inspect skin frequently, keep skin dry, ensure patients have access to the best nutrition and hydration, and help and encourage patients to move frequently.
This is very important in maintaining quality care as pressure injuries can cause significant pain and discomfort that can slow a patient’s recovery.
We achieve this rate through an established Pressure Injury Prevention Management Program and the reporting and monitoring of every pressure injury for the purposes of identifying areas for improvement.
The graph below shows the number of patients who developed a pressure injury while at Euroa Health.

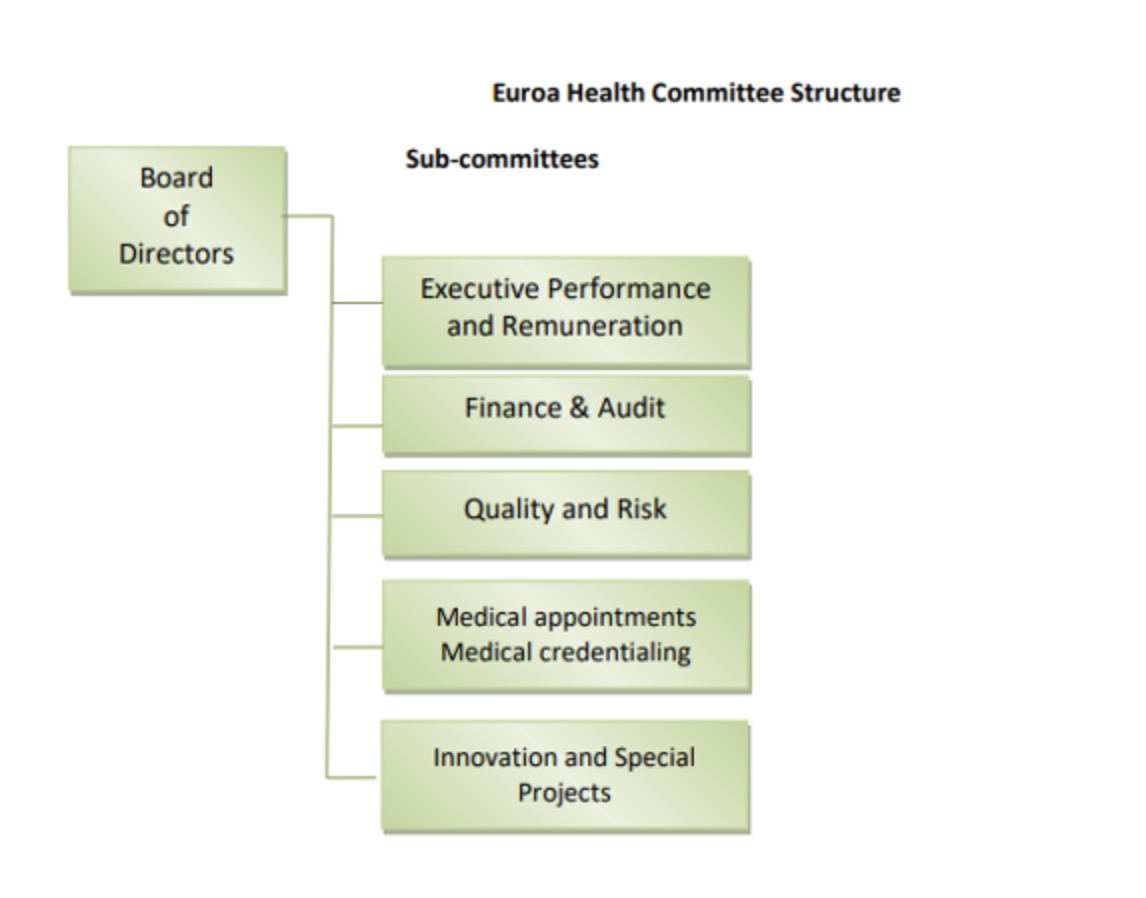
Adverse Blood Transfusion Events
As part of a hospital admission, you may require a blood transfusion, which is a procedure where you receive blood through your vein. Blood transfusions may be necessary for several reasons, for example, if you are anaemic or if your body is not producing sufficient blood cells. Blood transfusions can be a lifesaving measure but is not without some risk and therefore is only prescribed after a doctor has deemed it necessary.
We achieve this by ensuring blood is only prescribed when necessary; ensuring staff are competent in blood transfusion management; and by ensuring that blood and blood product usage is in line with current best practice guidelines, as set out by the National Standard for Blood and Blood Products.
Blood Management Standard | Australian Commission on Safety and Quality in Health Care
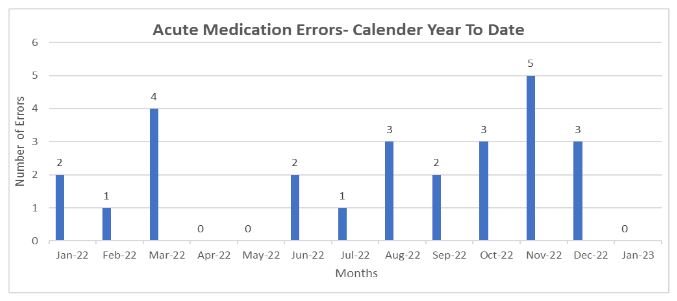
Medication Errors
Each month Euroa Health identifies the number of medication errors occurring in the processes of prescribing or administration of medication. The graph below shows the number of medication errors per month for the service.
Patient Experience Data
In 2021 Euroa Health commenced the collection of patient experience data to provide us with an insight into the ways in which patients view their experience of a number of non-clinical and clinical aspects of care.
These measures not only enable us to have a better understanding of how each patient perceives our quality of care in real time, they also provide the opportunity for us to act on any feedback or concerns straight away in partnership with them. The data collected is then used to inform our Quality and Improvement program. An example of the data in graph form is shown below
Standard 5 – Acute Audit (New), all figures % of patients surveyed
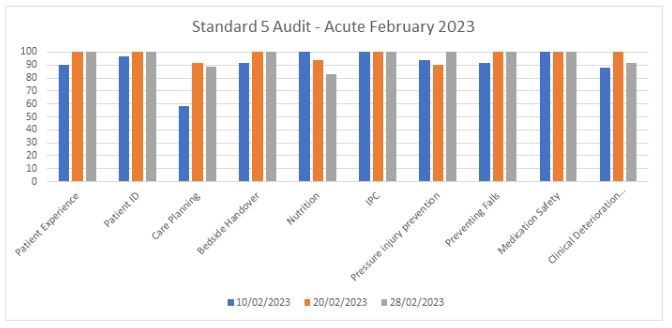
Patient Experience – is the patient happy with their room, quality of food, cleanliness of facilities, have they had their clinical journey and discharge plan explained to them, are they delighted with their experience at EHI and any suggestions for improvement.
Patient Identification – is the patient wearing a legible and current identification band and does it identify any allergies, are they asked for 3 points of ID prior to any procedures or medications.
Care Planning – was the patient included in planning their treatment and care, were they included in planning for their discharge from hospital.
Bedside Handover – were clinical staff change of shift handovers performed at the patient’s bedside, were they included in the handover process and given the opportunity to provide input, was their communication board updated for their benefit.
Nutrition – is the patient at risk of malnutrition, have they a choice in their nutrition plan, are weights recorded.
Infection Prevention and Control – did staff observe the 5 Moments of hand hygiene 100% of the time, do all staff wear gloves, are all cannulas or catheters clean and are they changed regularly.
Pressure Injuries – have they had a skin assessment, have they been advised on best methods to avoid PIs, if confined to bed do staff regularly assist with position changes.
Medication Safety – have patient’s allergies been discussed with them, are they asked about them when receiving medications, have they had an opportunity to discuss any concerns about medications with their doctor or a pharmacist, are any medication changes explained to them.
Clinical Deterioration – does the patient (and family) know and feel confident using the procedure for escalating their concerns if they are worried about their health.
Acute Quality Systems
Quality Framework
A strong commitment to safety and quality underpins everything that we do.
We strive to deliver safe environments and systems of work to support our healthcare professionals in providing the safest possible care. We achieve this through a strong clinical governance framework.
Clinical Governance
Clinical Governance is the system by which Health Care Managers and clinicians share responsibility and are held accountable for patient safety, minimising risks to consumers and for improving the quality of clinical care. We actively seek patient/consumer feedback and participation, to assist us to continually improve our services.
The framework structure consists of key organisational elements to effectively improve the quality of healthcare we deliver:
- Governance, leadership, and culture
- Community and consumer involvement
- Competence and education
- Information/knowledge management and reporting
The Quality and Risk Subcommittee, reporting to the Board of Management, is responsible for monitoring and improving performance against standards, the identification and mitigation of risk, and compliance with legislation and contractual obligations.
It consists of 10 members and comprises consumer representatives, Board members, medical professionals and EHI executive
SCV Clinical Governance Framework.pdf (bettersafercare.vic.gov.au)
Mandatory Training and Performance Reviews
Euroa Health recognises that ongoing education is an integral component of our Quality and Safety policy. All staff undergo mandatory training each year as a condition of their employment, which includes:
- Infection Prevention and Control
- Hand Hygiene
- Basic Life Support
- General Evacuation
- Fire Awareness and Extinguisher Training
- Manual Handling
- Medication Calculations Competency
- Open Disclosure and Management of Adverse Events
- Bullying and Harassment
Staff participate in annual performance and development reviews with their manager, discussing achievement of set goals and planning the coming year. In addition to their mandatory training, staff are encouraged to advance their skills with a range of on-line, in house and externally provided education.
Private Hospital Patient Charter
Private patients’ hospital charter | Australian Government Department of Health
Euroa Health Open Disclosure Policy
Medical and Allied Health Credentialling
Euroa Health has an obligation to ensure Medical, and Allied Health Practitioners meet the credentialing and scope of practice requirements to practice safely and within their scope of experience, knowledge, and skills.
Credentialing refers to the formal process used to verify the qualifications, experience, professional standing and other relevant professional attributes of medical and allied health practitioners for the purpose of forming a view about their competence, performance and professional suitability to provide safe, high quality care services within the organisation.
In addition, all Medical, Allied Health and Nursing clinicians must have current registration with the Australian Health Practitioners Regulation Agency (AHP)